Vasectomy Reversal Surgery
Microsurgical Vasectomy Reversal Surgery in Sydney
Microsurgical vasectomy reversal (vasovasostomy) surgery is now available in Sydney. This is a minor surgical procedure used to undo a prior vasectomy and reconnect the tubes (vas deferens). Microsurgery uses sutures that are finer than human hair, and the reversal procedures is performed using a powerful microscope.
After a successful vasectomy reversal, sperm are again present in your semen and you may be able to get your partner pregnant. Dr Derek Lok is an eminently experienced Vasectomy Reversal Surgeon consulting and operating across Sydney. He has 25+ years of experience performing vasectomy reversal surgery and one of the highest case volumes of any surgeon in Australia performing vasectomy reversal surgery.
Watch the Procedure
How the Procedure is Performed
Steps to Performing the Microsurgical “Minimally Invasive” Vasectomy Reversal Technique.
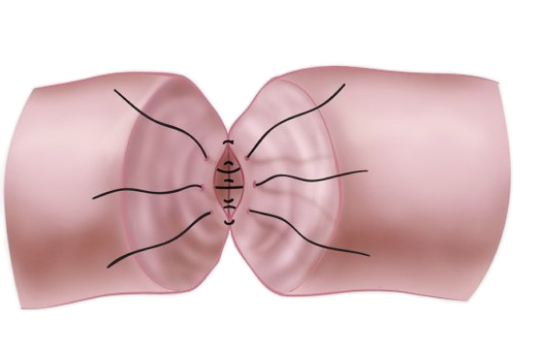
Step 1
Inner (mucosa) layer is stitched together.
Step 2
Outer (mucosa) layer is stitched together.
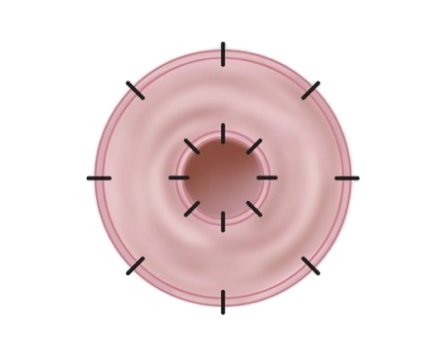
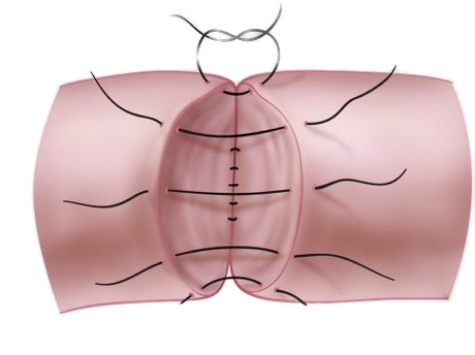
Step 3
Cross section showing placement of stitches.
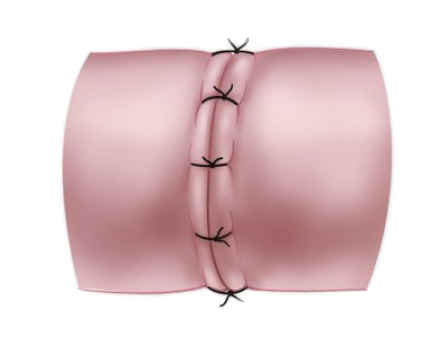
Step 4
Completed vasovasostomy.
A Gentle Approach to Vasectomy Reversal Surgery
The use of a microscope means smaller incisions, which means less tissue trauma. The microsurgical approach involves a single midline, or two 5mm “keyhole” small scrotal holes, similar to when the initial vasectomy was performed (but often smaller in reversal surgery as done by a microsurgeon while initial vasectomy often done using scalpel or scissors). *See photos further down page.
The previous vasectomy site is dissected with the dead scar tissues removed (we don’t leave lumpy tissues behind), the tied-off part identified and excised, the ends refashioned, and patency of each lumen tested.
The vas deferens openings, which have a diameter less than ½ a millimetre, are re-joined in two overlapping layers (as per above 4-step process diagrams) using a microscope, achieving an equivalent water-tight seal with sutures that are hardly visible to the naked eye (magnified under operative microscope up to 40x of normal vision) with very fine 8-9 O sutures, without the use of clamps (so as to minimise tissue handling and trauma).
Results
The microsurgical approach is superior to open surgery in vasectomy reversal surgery.
The Vasovasostomy (vasectomy reversal) Study Group (ASRM) found that with microsurgical techniques, sperm appears in the semen of 85-90% of men and 50-70% of their wives become pregnant; while with less ideal approaches (eg: open surgical approach still practiced commonly in Sydney by some surgeons), also results in sperm appearing in the semen of about 80% of men, only 20-40% of their wives conceive. Thus, the open surgical approach has a lower success rate of getting the female pregnant.
The experience of your surgeon matters:
The success rates of vasectomy reversal correlates with the operative frequency. A number of studies reported that surgeons who operate at high frequency of >= 15 vasectomy reversals per year reached a cumulative patency rate of 70% and a pregnancy rate of 33%; while those operate with a comparably low frequency of <= 6 cases per year obtained a cumulative patency rate of 45% and a pregnancy rate of 8.8% only.
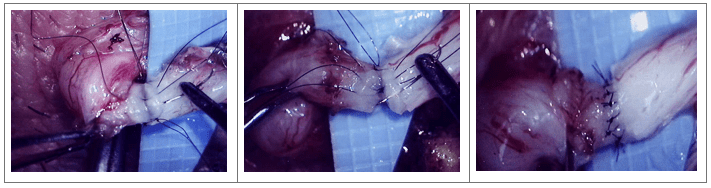
Photos of the Vasectomy Reversal Procedure
*Warning: graphic content of vasectomy reversal and male anatomy shown when opened.
Photos: The microsurgical vasectomy reversal
Either a single midline, or occasionally two 5mm “keyhole” small scrotal incisions are made to gain access to the vas deferens. After healing, the surgical incision is almost invisible. Below shows Dr Lok’s single midline incision where he performed vasectomy reversal on a patient.


Using the aid of a powerful microscope, vasectomy reversal surgery can be performed through a small keyhole with great accuracy when performed by an experienced surgeon. This is advanced microscopic surgery and the evidence shows that experience does result in improved surgical outcomes for patients.
Example of another doctors’ post surgical scaring from ‘open surgery’ technique, which failed, when compared to Dr Derek Lok’s keyhole vasectomy reversal surgery he performed on the patient to correct previous failure from elsewhere.

Advantages of Microsurgical Vasectomy Reversal Technique
What are the advantages of the microsurgical vasectomy reversal technique over the “open” method still practiced by some surgeons around Sydney?
- Higher chance of successful operation (compared to open technique) and thus, higher chance of conception
- Minimally invasive approach
- Small incision and thus smaller scars, and no need for a drain to remain implanted post-surgery
- Reduced pain and post-operative complications
- Meticulous overlapping, double layer re-join using very fine sutures
- Day surgery with same day discharge
- Rapid recovery and return to work
- Reduced costs
Dr Lok's Results vs. Public (Peer Reviewed) Results
Seven published series on vasectomy reversal surgery included a total of 2,330 patients who were available for follow-up, and these showed an average patency rates of 88% and pregnancy rate of 62%.
Dr Derek Lok’s own audit of 120 male patients operated on over 3-years, with follow-up for up to 3-years, has demonstrated the presence of sperm in the ejaculate following surgery in 90% of patients, beating the average as per the peer reviewed studies.
About Your Surgeon
Vasectomy Reversal Surgeon
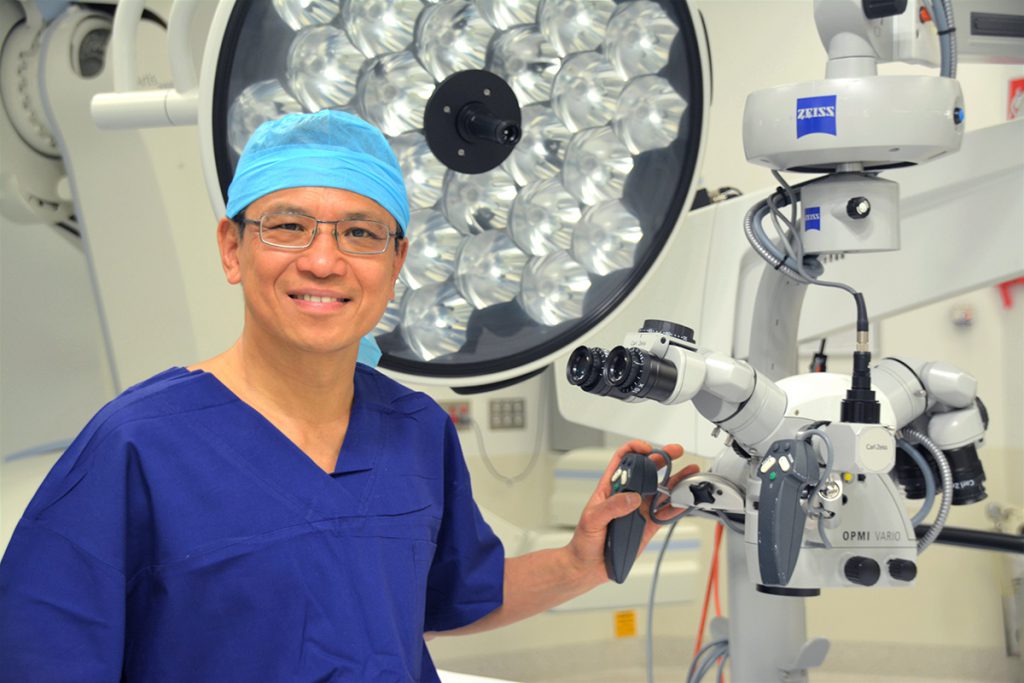
Dr Derek Lok
MBChB, PhD, FRANZCOG, CREI
Dr Lok is a Sydney-based Specialist Obstetrician & Gynaecologist and Fertility Sub-Specialist, with a sub-specialist interest in advanced microsurgery. He offers 25+ years of experience performing vasectomy reversal surgery.
Dr Derek Lok is a sub-specialised microsurgeon who performs the meticulous microsurgical vasectomy reversal procedure. He offers tremendous experience, having performed close to a thousand of these advanced procedures. He consults and operates across Sydney.
Factors That Influence A Successful Outcome
The Interval Between the Initial Vasectomy and Reversal Surgery
The increase in pressure, which results from tying off the vas, is transmitted to the much finer and thin walled duct, which attaches to the vas called the epididymis (around 6 meters long). After variable periods of time (about 10-15 years following original vasectomy), the dilatation may cause a rupture or a “blowout” of the duct leading to a blockage.
Because it is a single duct, sperm will no longer reach the site where vasectomy was performed. Re-joining the vas under these circumstances will not be successful as the rupture site(s) are difficult to identify and often bilateral. Ruptures rarely cause symptoms and are not easily diagnosed by examination or imaging.
Finding the spontaneous flow of fluid when the vas is open at reversal is a good but not absolute prognostic sign for a successful outcome. The presence of live sperm in the fluid of the opened vas is the best finding for success.
The Vasovasostomy Study Group (ASRM) found that in 1,247 patients the patency and pregnancy rates to be 97% and 76% if the obstructive interval was less than three years, 88% and 53% if three to eight years, 79% and 44% if nine to 14 years, and 71% and 30% if 15 years or longer.
Sperm Antibodies
Particularly in the first two years after vasectomy it is not unusual to find the presence of “antibodies” to sperm in blood tests. When persistent in high levels in later years they may interfere with sperm function by causing sperm to clump or stick together following ejaculation thus interfering with their ability to fertilise oocytes (the female’s eggs).
Tests on ejaculated sperm give the best indication of the significance of sperm antibodies and overall their presence is not a contraindication to surgery, as often antibody levels drop once the continued leakage or challenge to immune system is eliminated after flow restored by reversal surgery. Hence the majority of reversal surgeons are not currently carrying out antibody tests before surgery.
Post-Reversal Sperm Quality
Frequently Asked Questions
When can I have sex after vasectomy reversal surgery?
How do I know if the operation has been successful and how long does it usually take to conceive?
What complications can occur?
Do you need to request any specific tests if you want the option to reverse it?
Cost of Vasectomy Reversal Surgery
We regard ourselves as a medical service, not a commercial business. We charge according to the complexity and length of the surgery, in line with Australian Medical Association (AMA) recommended Fees.
Surgeon's Fee
Anaesthetist's Fee
Hospital Fees
Insured Patients:
If you have private health insurance, depending on your policy, your hospital fees should be fully covered by your your health fund.
You should contact your health fund prior to surgery to confirm you are covered for this procedure.
Uninsured Patients:
If you do not have private health insurance, you are liable to pay the hospital fees out-of-pocket.
Genea Day Surgery in the Sydney CBD offers competitive pricing for the procedure, currently $2,992. It is best to contact Genea for current pricing should you wish to proceed.
Surgical Booking Payment:
A payment is required 2-weeks prior to the date of your operation to confirm your place on Dr Lok’s operating list (or at the time of confirmation of date of surgery if booking is made less than 2 weeks before your operation).
A cancellation fee of $500 is payable for cancellation of surgery less than 2 weeks prior to the date of operation. This amount will be refunded if a future booking for surgery is made.
When & Where:
Dr Lok has a few operative lists every week, including some Saturdays, and will be able to fit you in within a week or two at one of the following Day Surgery and Hospitals:
- Genea Day Surgery (Sydney CBD)
- Strathfield Private Hospital (Strathfield, NSW)
- Sydney South West Private Hospital (Liverpool, NSW)
- Mater Hospital (North Sydney, NSW)
Have a Question or Enquiry?
If you have a question or enquiry related to vasectomy reversal surgery, please get in touch and we will get back to you.
